How to access medicinal cannabis in Australia

Patients have been left wondering how they can access medicinal cannabis in Australia…until now.
Despite the Australian government approving the use of cannabis for medical purposes close to three years ago, there is still some red tape in the way of Australians getting access to the drug.
A lot of the information out there can be vague and confusing and it can seem a little overwhelming.
You have a medical condition, or maybe your child is sick, and you just want to obtain a more natural but clinically proven treatment without turning into a criminal for it.
Australian medicinal cannabis ancillary services provider Cannvalate’s chief executive officer Dr Sud Agarwal gave Small Caps the lowdown on exactly how access works in Australia.
Where can you get medical cannabis in Australia?
In October 2016, the Narcotic Drugs Amendment Act 2016 came into effect in Australia, allowing doctors to legally prescribe medicinal cannabis to patients with specific medical conditions through the Therapeutic Goods Administration (TGA)’s Special Access Scheme.
Dr Agarwal said since legalisation occurred, there has been an increased “softening of the regulations to prove eligibility for medical use”.
“It’s federally open – it’s the same essentially everywhere [in Australia],” he said.
“Some people say there’s a patient access problem but it’s not really a government problem anymore; it’s more a function of cost or efficiencies of the system,” Dr Agarwal added.
Getting a prescription
As you are probably aware, medicinal cannabis is not an over-the-counter medication and you need a very restricted prescription for it.
However, Dr Agarwal said the “biggest myth” about the authorised prescriber scheme is that doctors need to be preapproved by the TGA to prescribe medicinal cannabis to patients.
“Any doctor can prescribe it now – GP or specialist,” he said.
“The vast majority of prescriptions, probably 98%, are not prescribed by authorised prescribers. It’s probably the biggest misconception. They’re prescribed by regular doctors under the Special Access Scheme,” Dr Agarwal explained.

Dr Sud Agarwal is an internationally recognised key opinion leader in the clinical use of cannabinoid medicines.
Still, it’s not as simple as popping to your GP and being issued a script – you need to have your medical condition verified as being appropriate for the treatment.
“The doctor makes an application to the TGA to certify that it’s a condition that would be an appropriate use of cannabis and that the product the doctor selected is an appropriate one too,” Dr Agarwal said.
“Usually there needs to be some form of clinical justification, which is usually done by attaching some form of medical literature evidence. Once you’ve got that, within very short period of time, the TGA will confirm: yes, it’s approved, or no, we need further information.”
Dr Agarwal said the process is “usually very quick now”.
“It used to take weeks or months – now it’s often the same day or next day approved,” he said.
According to the TGA, 2893 Special Access Scheme Category B applications were approved in August 2019. This is almost 12 times more than the 229 approvals recorded in August 2018.
Who can be prescribed medical cannabis?
The medical conditions that cannabis can be prescribed for is quite extensive – but you can’t use it to treat the common cold.
Clinical trials and medical research has shown medicinal cannabis can assist in the treatment of symptoms for conditions including but not limited to: chronic pain syndrome; neurological conditions such as epilepsy; multiple sclerosis and motor neuron diseases; inflammatory bowel diseases, Crohns disease and ulcerative colitis; chronic cancer pain and malaise; chemotherapy-induced nausea and vomiting; arthritis; and dementia.
Dr Agarwal said chronic pain is the most common reason medicinal cannabis is prescribed, followed by neurological illnesses and inflammatory diseases.
“Then, a lot of people are in between where they have a primary disease that has led to prolonged or chronic pain and they’re now taking it for that condition, in conjunction with their chronic pain medication,” he added.

Medicinal cannabis is most commonly prescribed for patients who suffer from chronic pain.
In addition, the majority of medical cannabis use is as an adjuvant, which helps to improve the efficacy of other drugs. This means it can enable a patient to lower the dose of their existing medication so they are not suffering the same level of side effects.
According to Dr Agarwal it is “not uncommon” for patients to take medical cannabis in conjunction with their pain meds and “reduce their total opiate dosage by 50%”.
“We have seen people who are taking anti-inflammatory medication, such as steroids like prednisolone, for inflammatory conditions like rheumatoid arthritis or inflammatory bowel disease and they have reduced their steroid dose by 30%,” he added.
How easy is it to be approved?
Despite anecdotal stories of people being rejected by the TGA and ‘forced’ to obtain cannabis elsewhere (i.e. illegally), Dr Agarwal said it is not too difficult to be approved but conceded there is an “art” to writing the TGA justification letter.
“I think it would be unheard of for somebody who is a bona fide candidate to get disapproved now,” he said.
If a patient is rejected by the TGA, there is usually a Request for Further Information issued and Dr Agarwal said he has never had somebody he thought was a bona fide candidate disapproved on the second round application.
He added there were no additional restrictions for prescribing medical cannabis for children, but it would be “entirely down to the doctor’s discretion” to make sure he has appropriate parental monitoring and safety checks in place.
“The doctor would need to be more mindful about dosing it and about what the effects will be. The most common concerns that doctors have is that they’re going to overly sedate the patient and that they are going to stop breathing.”
“I’m an anaesthetist by background so for me, this is not a real fear; but if you’re a doctor who doesn’t have experience with drugs of sedation, it may appear to be a more complex task,” Dr Agarwal said.
Getting the right dosage
According to Dr Agarwal, the most common “side effect” of medicinal cannabis is drowsiness. Another common side effect is tachycardia, that is where the heart speeds up.
He said there is a fine art in dose escalation, which many doctors can find “confronting” because medical cannabis is unlike conventional drugs such as paracetamol, where a standard dose is administered.
Every individual person has a different endocannabinoid system and one patient’s system’s sensitivity to cannabis could be different to the next person.
“I may be double your body weight, but it may be that you would need twice the dose as me because you might have an endocannabinoid system that is more resistant to cannabinoids,” Dr Agarwal explained.
“The only way to be absolutely sure – and this is what we do with all patients in my clinical practice – is we start with the lowest actual dose required that would be safe on the most sensitive person.”
“We recognise that 90% of the people will not feel any benefit from that, and this is where people have tried cannabis and said it’s never worked for them, but they’ve probably just been underdosed,” he said.
The dose is then doubled every day or second day until a therapeutic response is achieved.
“As long as the patient is having an appropriate therapeutic response to the underlying pathology without incurring any side effects, then we’ve found our therapeutic window.”
“The thing is, your therapeutic window and the next person’s could be entirely different – it could be by a multiple of five,” Dr Agarwal said.
Does medical cannabis contain THC?
Depending on the condition being treated, prescriptions could be for pure cannabidiol (CBD) or CBD plus tetrahydrocannabinol (THC), which is the psychoactive ingredient associated with producing the euphoric effects of cannabis.
Dr Agarwal said in the case of paediatric epilepsy, patients tend to be prescribed a pure CBD mixture.
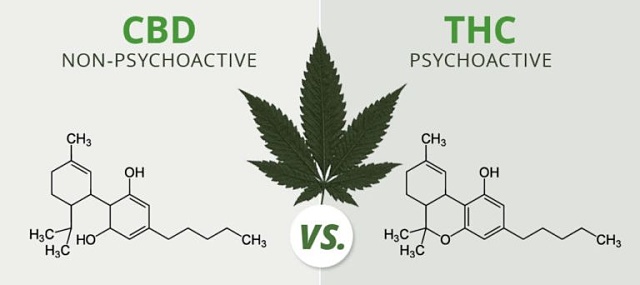
CBD vs THC
However, in the case of chronic pain, some THC would assist.
“Some people might have more THC than CBD – it might be a 1:5 ratio. It depends what underlying pathology you have,” he said.
Filling the script
So, now that you’ve got the prescription with the TGA approval stapled to it, you can go to any pharmacy to get the script filled.
Dr Agarwal said a pharmacy near the patient can organise for the product to be despatched from Cannvalate’s warehouse to wherever they live in Australia.
“We’ve got just over 600 pharmacies now in our network and 98% of the population should have to go less than 2km as most people live in urban areas with a pharmacy nearby,” he said.
Cost and subsidisation
Unlike most medicines in Australia, medicinal cannabis is not subsidised under the Pharmaceutical Benefits Scheme.
Victoria has a compassionate access scheme that funds medicinal cannabis products for a limited number of children with severe epilepsy, while New South Wales’ scheme can be granted for adults with terminal illnesses.
However, Dr Agarwal said “under 1% of patients” use these schemes and they receive “compounded, non-branded” products.
As Cannvalate allows any manufacturer to sell through its network, the company doesn’t control the pricing.
However, Dr Agarwal said the typical “ballpark figure” was between $200 to $600 per month.
“It is expensive. Having said that, only of recent times – as in the last few weeks – there’s now cheaper products from Colombia and Lesotho [a small country landlocked inside South Africa], which are much lower-cost products,” he said.
Medical cannabis vs homegrown
So, what’s to stop the ordinary Australian from growing their own?
The most obvious reason is the criminal implications. Cultivating illegal cannabis is still a serious offence in all states and territories of Australia.
Depending on the severity, penalties can range from large fines right up to life imprisonment.
Dr Agarwal said another important difference is that the dose is known and when you get medical cannabis from a doctor, it’s “infection-free” because it has been packed in a sterile manner.
In addition, he said it has been manufactured under the Goods Manufacturing Practice, which means “someone has certified it does not contain heavy metals or bacteria and each dose you get contains the same amount of active ingredient every time”.
“If you crush some bits of a plant, what you take on Monday might be different to Tuesday”.
“Generally, with medicines, you want to get the safest dose that allows you to achieve your desired therapeutic effect without side effects. I can’t see you achieving that with plant dosing very easily,” Dr Agarwal added.
The next generation of medical cannabis products
Dr Agarwal said it was important for Cannvalate to be multi-faceted in the cannabis industry since it is a relatively early-stage industry where people need a lot of different services.
In addition to its distribution network, which covers around 40% of all prescriptions in Australia, it has a research division that is currently running 12 clinical trials for a range of indications.
Some of those trials are with Impression Healthcare (ASX: IHL), of which Dr Agarwal was recently appointed as the chief medical officer.
Dr Agarwal said the most exciting aspect of the company is its “novel cannabinoid drug discovery” division, which is only about four months in the making.
This arm involves developing novel cannabinoids using a mixture of ingredients and validating them for specific diseases.
Dr Agarwal called it “Cannabis 2.0 – a unique product for a unique disease”.
He said at the moment people are buying generic cannabis oil where it doesn’t matter what company you’re getting it from, but the next generation of cannabis products will need to be more disease-specific.
If Cannvalate can develop a lead candidate, it will be a derisked product than will have been shown through trials to work better than regular, generic cannabis.
In addition, the dosing will be “tighter” because it will be clinically validated and measured in controlled experiments to be effective at very specific target receptors in the human body.
This could mean far less trial and error when it comes to patients finding a dosage that is suitable for their condition, which is reassuring for both patients and their prescribing practitioners.
