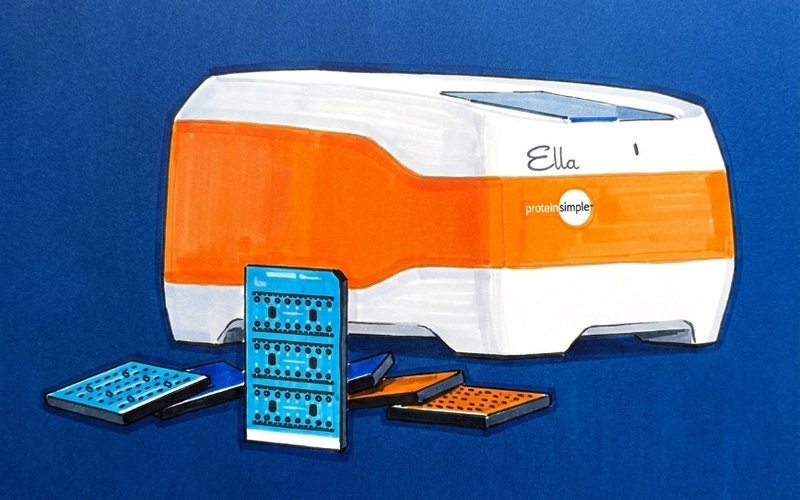
Cleo Diagnostics (ASX: COV) has selected the Ella automated enzyme-linked immunosorbent assay (ELISA) platform to deliver its ovarian cancer technology to market.
Developed by American life sciences company Bio-Techne Corporation, Ella has been designed to deliver accurate, reproducible data with reduced manual input, as well as offer materially improved assay sensitivity, precision, and automation.
The platform also has the ability to simultaneously analyse multiple biomarkers compared with conventional ELISA platforms.
Patient blood samples from within Cleo’s ovarian cancer test kits will be processed in a laboratory on the Ella platform using microfluidic cartridges to measure Cleo’s proprietary biomarker panel, which form the key inputs of the algorithm underpinning its patented technology.
Platform Capabilities Confirmed
Cleo commenced using Ella in September, and has confirmed the platform’s capability to deliver its ovarian cancer technology.
The companies are now in advanced discussions on a formal binding agreement for Bio-Techne to employ Ella for the analytical validation of Cleo’s kits
Those kits will then be used test approximately 500 blood samples collected as part of the company’s pivotal clinical trial.
The results will form the primary data package for its upcoming 510(k) submission to the US Food and Drug Administration.
Cleo and Bio-Techne are also preparing to enter into a long-term commercial supply agreement once these activities have been completed.
Accurate and Early Diagnosis
Cleo is developing a simple blood test for the accurate and early diagnosis of ovarian cancer based on the novel patented biomarker CXCL10, which is produced early and at high levels by ovarian cancers but is largely absent in benign forms of the disease.
The test aims to distinguish benign from malignant growths in a standard format that will be readily compatible with existing equipment used by diagnostic laboratories worldwide.
Cleo’s technology is backed by over 15 years of scientific research and development at the Hudson Institute of Medical Research in Victoria, with two clinical studies conducted on more than 500 patients.
A benchmarking study in 2024 showed the test could correctly detect 90% of early-stage cancers compared to the 50% success rate of standard clinical workflows that use cancer antigen 125 testing and ultrasound to predict malignancy.